In the dynamic landscape of healthcare, the quest for innovation never ceases. While strides have been made in leveraging AI for backend processes, there’s a growing appetite among healthcare teams for AI solutions that directly impact clinical workflows and elevate patient outcomes. Enter AI-enhanced telehealth—an exciting frontier where cutting-edge technology meets compassionate care.
Picture this: A hospital equipped with state-of-the-art telehealth services, seamlessly integrating AI capabilities at the point of care. This isn’t just a vision of the future; it’s the reality of modern healthcare.
The evolution of telehealth endpoints has been nothing short of remarkable. From basic audio interactions to immersive video encounters, the quality of cameras and microphones has soared, mirroring the advancement of technology itself. But what sets today’s telehealth apart is the integration of edge computing—a game-changer that brings AI to the forefront of patient care.
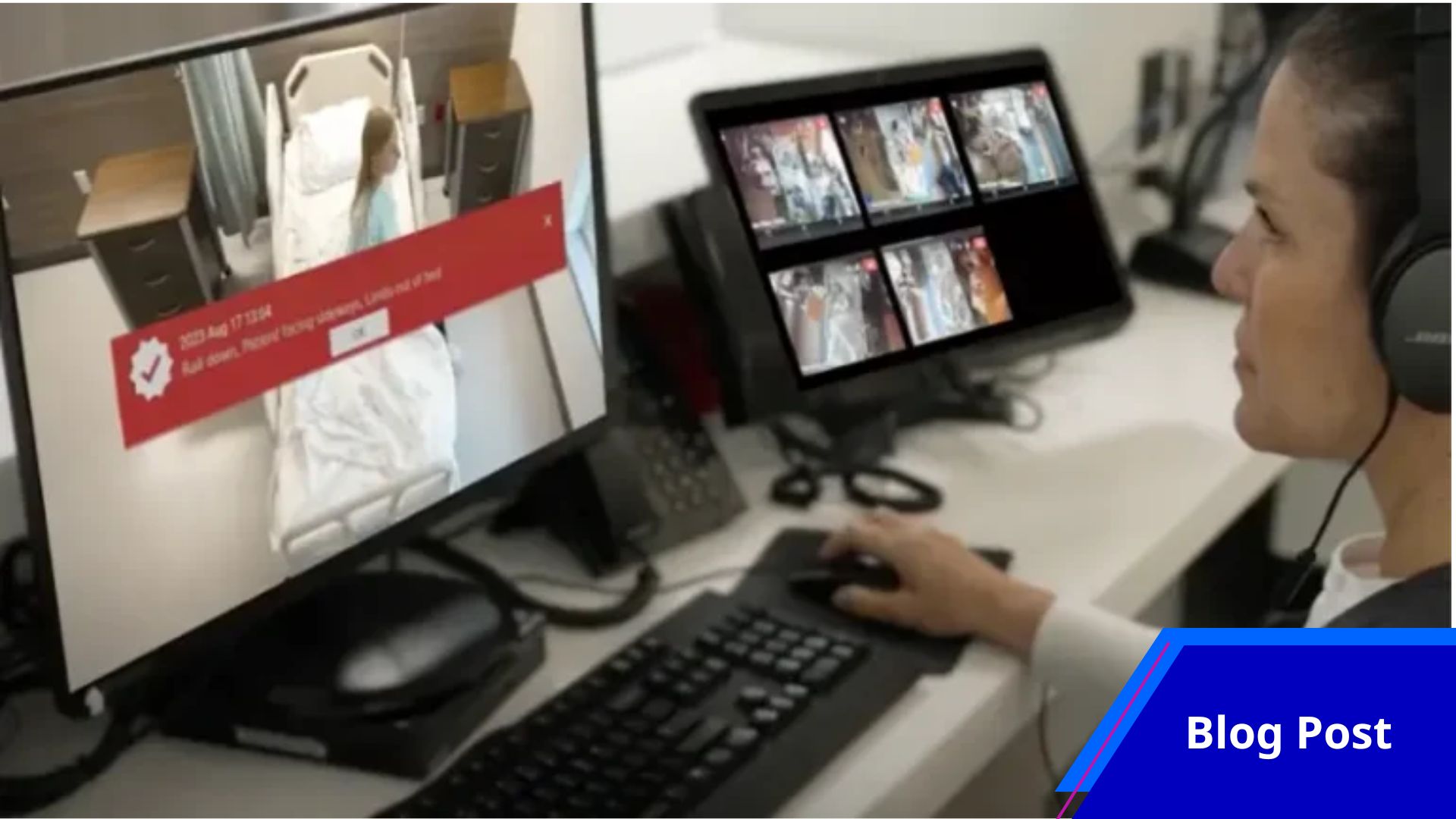
Imagine multiple cameras capturing every detail, allowing care teams to engage with patients virtually while simultaneously tapping into powerful AI solutions. This isn’t science fiction; it’s the new standard in telehealth innovation.
And it doesn’t stop there. Emerging sensor technologies are seamlessly woven into telehealth platforms, silently capturing vital clinical data without disrupting the care process. These innovations pave the way for AI-powered services like Augmented Observation and Vitals Trending—tools that not only enhance patient safety but also alleviate the burden on healthcare staff, leading to superior outcomes.
In this era of AI-enhanced telehealth, the bedside becomes a nexus of innovation and empathy—a place where cutting-edge technology and compassionate care converge to transform lives. Welcome to the future of healthcare.